Prosthesis is the name given to the device that imitates the function of the missing or inadequate organ or limb of the body. Arthroplasty or joint prosthesis surgery is the process of surgically removing the articular cartilage that cannot function adequately and replacing it with an artificial joint surface. Joint prostheses should not be confused with prostheses used to create images and provide function after limb amputations (eg externally attached devices to enable walking in case of leg amputation).
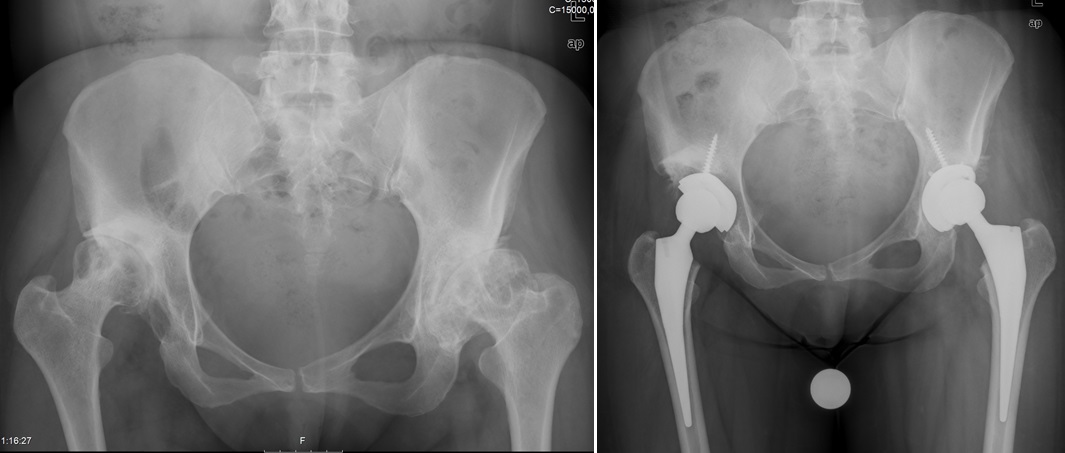
It is possible to summarize the procedure performed in arthroplasty surgery as follows: In joints that cannot be repaired, the articular cartilage, whose integrity is completely broken, is cut out to include some of the bone tissue underneath, and an artificial joint is created by placing metal materials with high tissue compatibility with or without bone cement. . Joint prostheses usually consist of two metal parts and a plastic part between them. The aim here is to imitate the natural, slippery and functional movements of a healthy joint by creating a new artificial joint. Arthroplasty interventions are among the most frequently performed surgical interventions in the discipline of orthopedics and traumatology.
WHICH JOINTS IS ARTROPLASTY SURGERY APPLIED?
Today, it is possible to surgically replace many joints. These are mainly hip and knee joints, shoulder, elbow, ankle, wrist, spinal disc and finger joints.
IN WHICH ORTHOPEDIC DISEASES IS ARTROPLASTY SURGERY PREFERRED?
Joint calcification (osteoarthritis) is the leading cause of application of joint prosthesis surgery. Articular calcification is a chronic joint disease that progresses with pain, deformity and loss of function as a result of damage to the joint surfaces due to various reasons. Osteoarthritis, which is common over the age of 40, is one of the diseases that limit the freedom of movement of the person. It shows the severity of the disease in direct proportion to the destruction of the joint and the wear on the cartilage surfaces.
Apart from calcification, intra-articular fractures that cause cartilage wear, diseases that cause deterioration of joint alignment, diseases that cause joint inflammation such as rheumatoid arthritis, congenital or developmental diseases that disrupt the structure of the joint, bone death (osteonecrosis) and cause constant pain that cannot be achieved with other treatments. Arthroplasty surgery can also be applied in many diseases that cause disease.

WHAT ARE THE COMPLAINTS OF PATIENTS WHO ARE PLANNED FOR PROSTHETIC SURGERY DUE TO CALCIFICATION DISEASE?
The main requirement of prosthetic surgery is that the patient feels joint pain. Due to pain, patients experience limitations in daily functions, decrease in joint movements, and difficulties in walking and climbing stairs. While pain occurs only with strenuous physical activities in the early stages, pain at rest at night may develop in the later stages. Over time, deformities in the joints can be added to the table. Although the duration of the complaints usually spreads over many years, sudden increases in pain intensity can be observed. The disease can sometimes progress without any symptoms.

WHAT ARE THE TREATMENTS THAT CAN BE APPLIED IN CASE CAUSED TO JOINT Calcification?
First of all, the cause of the pain is investigated and pain and functional limitations are tried to be eliminated with non-operative treatments. Treatment can be done with drugs (pain reliever-analgesic and edema solvent-anti-inflammatory) and physical therapy applications in the early stages of the disease. Patients should be advised to lose weight. In order to control the complaints related to the disease, intra-articular cortisone injections, joint fluid imitating (hyaluronic acid) or regenerative (platelet-rich plasma-PRP) injections are useful applications in the early stages. Supplementary drugs (glucosamine and chondroitin preparations) taken orally and supporting the cartilage tissue also help in the early stage treatment.
In the late stages of the disease, the above-mentioned treatments are insufficient. In this case, surgical treatments come to the fore. In surgical treatments, there are many different treatment options, from arthroscopic surgeries (see; Arthroscopic surgery), to bone osteotomy surgeries (surgery in which angular corrections are made by cutting the bone), and finally to joint prosthesis surgery, depending on the degree of joint damage and the functional status of the patient. Deciding which surgical intervention will provide the most benefit is the key to success. Joint prosthesis surgeries are in the last place among the surgical options mentioned above. If there is no response to the treatments applied after all methods have been tried, prosthesis surgery is preferred.
AT WHICH AGE GROUP SHOULD ARTROPLASTY SURGERY BE PREFERRED?
Arthroplasty surgery should not be applied to young patients except in mandatory cases, and joint cartilage-sparing treatment methods should be preferred in these patients as much as possible. It can be said that the lower age limit for which arthroplasty surgery is generally preferred is 60 years old. In the past, when prosthesis technology was not as developed as it is today, it was recommended to perform this surgery at as advanced ages as possible, since the life of the prosthesis was not long enough. However, since today’s technology produces prostheses that are more compatible with the human body, more durable, longer-lasting and allow more movement, prosthesis surgery can be performed when necessary, starting from the age of 50. It may be thought that arthroplasty surgery will be risky at very advanced ages and that patients will not be able to handle a major surgical intervention. An exact age cannot be specified as the upper age limit. If the patient’s systemic diseases are not dominant and the risk factors to be evaluated before the surgery for the surgical intervention are not clear, it can be said that arthroplasty surgery can be applied in every age group, considering the pain, loss of function in daily life and expectations of the patients.
HOW ARE PATIENTS EVALUATED BEFORE ARTROPLASTY SURGERY?
Additional systemic diseases (diabetes, heart failure, coronary artery diseases, lung and kidney diseases) that may occur in advanced ages increase the risks of arthroplasty surgery. For this reason, after prosthetic surgery is decided, the patient is evaluated with detailed examinations and additional problems are determined, and if these additional problems increase the risk of surgery very seriously, the pros and cons of the surgery are reviewed and a decision is made. There are also some increased risks in overweight patients due to the fact that additional problems (diabetes, high blood pressure, heart diseases) are more common.
WHAT IS DONE BEFORE AND AFTER THE SURGERY?
After the surgery decision is made, the patients are prepared for anesthesia. Anesthesiologist should be informed about additional diseases, drugs used and subjects that are considered important for the patient. If anti-coagulant drugs such as Kumadin, Plavix, Coraspin are used, doctors should be informed before hospitalization as they require special preparation.
Apart from the general examination, blood tests are performed, and heart electrocardiogram (ECG) and chest X-ray are taken. Preparations are made for blood transfusions that may be needed during or after the surgery. If the anesthesiologist deems it necessary, consultations from other departments (cardiology, chest diseases, internal medicine, etc.) are requested and a more detailed evaluation of the patient is carried out.
Arthroplasty surgery can be performed with epidural-spinal (a form of anesthesia performed through a needle from the lumbar region) or general anesthesia. Anesthesiologist decides the type of anesthesia. When epidural anesthesia is performed, a system is usually set up in which the patient can control his/her post-operative pain via a button. Apart from this, the pain associated with the surgery is relieved with medications. After the surgery, compression stockings are worn to prevent coagulation in hip, knee and ankle joint prosthesis surgeries.
On the day after the operation, when the patients’ general condition, blood values, blood pressure and heart rate are normal, they can be walked with the help of a walker. It is ensured that he gives full weight to the operated leg while walking. After standing up a few times, the patient can get up and walk around with a walker, sit on the toilet, and eat his meal while sitting on the sofa whenever he wants.
Patients are shown exercises that increase the movement of the joints they have operated on and strengthen them, and they are encouraged to repeat them throughout the day. Usually, no additional physical therapy is needed.
Antibiotic treatment is continued for 1-2 days after surgery. Anti-coagulant drugs are used for 2-4 weeks if there are no medical obstacles.
HOW ARE PATIENTS FOLLOWED AFTER DISCHARGE?
If there is no problem, patients are usually 4-6 days after surgery. day discharged. Patients who continue to walk with a walker and do their exercises at home should not touch the wound area with water until the stitches are removed. For patients who have undergone hip replacement, cross-legged movements where one leg crosses the other or sitting in low places such as Turkish style toilet should not be preferred.
Generally, the sutures are removed towards the end of the 3rd week and the patient’s condition is evaluated by performing controls at the 6th week, 12th week, 6th month and 1st year.
A doctor should be consulted immediately in cases of severe pain, fever, discharge at the wound site, bad odor, redness, swelling, inability to breathe, limitation of movement of the operated area or inability to step on it, other than normal controls.
Most modern prostheses are made of MR compatible metals. For this reason, there is no problem in performing MRI to areas outside the surgical field. Against the signals that may occur while passing through metal detectors, it would be appropriate to obtain a document explaining that you had surgery and the prosthesis used.
WHAT ARE THE RISKS OF ARTROPLASTY SURGERY?
In patients who are candidates for arthroplasty surgery, comorbidities with age may bring some risks for anesthesia and surgery. Infection (inflammation), clot formation in the veins and mechanical problems of the prosthesis are among the risks that can be experienced.
Infection is a problem seen at very low rates in good operating room conditions and with the use of preventive antibiotics. For this, it is ensured that there is no infection in another part of the patient’s body, if any, surgery is planned after treatment. In all patients, prophylactic antibiotics are given just before the operation and it is continued for a few days after the operation. The operating room conditions and the precautions taken by the surgical team against infection are very important in the fight against infection. Despite all these precautions, there is a small possibility that microbes from another part of the patient’s body may reach the joint area and cause infection in the prosthesis, both during and after the operation.
Clot formation in the veins is a problem that can be seen especially in patients with disorders that cause clotting tendency and long-term immobility. All patients are protected from this problem by administering drugs that prevent clotting for 2-4 weeks after surgery. In addition, this problem is tried to be avoided by allowing the patient to move and walk quickly after the surgery. Despite all the precautions, the formation of a clot in the leg veins and the fragments that break off from this clot, causing respiratory problems, especially by blocking the pulmonary vessels, are a rare problem.
Prosthesis-related mechanical problems (prosthesis dislocation, wear, loosening) are among the rarer problems today.
Apart from these, wound healing problems, less joint movements than expected, continuation of pain despite everything being found to be normal are other rarely seen problems.
The lifespan of prostheses used in arthroplasty surgery can extend up to 15-20 years. With a well-performed prosthesis surgery, satisfactory results are obtained for the patients. It is very important for the success of the surgery to inform the patients in detail before the prosthesis application. As with any surgical procedure, prosthetic surgery has its own risks. In order to minimize these risks and increase patient satisfaction, the following three conditions must be met:
The right patient, the right technical conditions and the right surgeon !!!
